Although rare in the general population, anal cancer is more frequent among HIV positive men and women. We know more about the rates among HIV+ men than among women. For example, HIV+ MSM are 80 times more likely to develop anal cancer than HIV- men. Anal cancer incidence is rising among HIV positive men and women despite effective treatments for HIV.
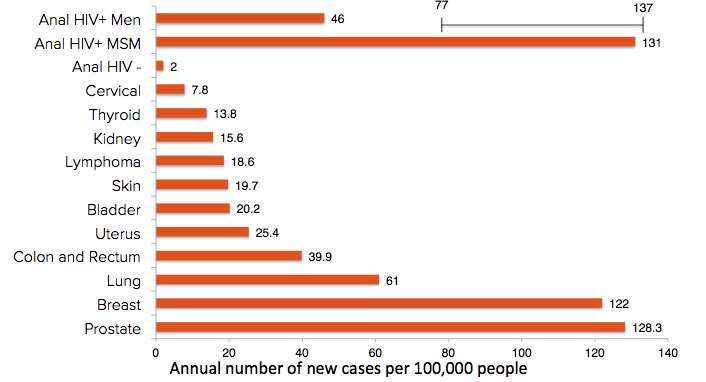
Rates of Anal Cancer Compared to Other Cancers
Cancer rates are usually measured as the number of cases of a particular cancer each year per 100,000 people. This number of new cases per 100,000 people is called the "incidence" rate. The incidence rates of the most common cancers are compared in the chart below. The first three bars show the very different rates in anal cancer among HIV positive men, HIV positive men who have sex with men (MSM), and HIV negative men. Estimates of the cancer rates for HIV + MSM are highest and range from 77 to 137. The anal cancer incidence rate among HIV positive MSM is even higher than the rates of much more common cancers that are routinely screened for in the general population.
Anal cancer is caused by Human Papillomavirus (HPV), which can cause changes to the skin around and inside the anus. These changes are called "high-grade squamous intraepithelial lesions" or (HSIL). About half of HIV+ MSM have anal HSIL. Not all anal HSIL will develop into cancer. Most HSIL will go away on their own, but a few become cancer and can spread to other parts of the body. The risk of developing anal cancer increases with age. HSIL do not cause symptoms, so by the time symptoms are noticed, cancer may have already developed.
We estimate that 1 in 10 HIV+ MSM will get anal cancer over their lifetime. The story for HIV+ women is even less clear. We estimate that 2 or 3 of every 10 HIV+ women have anal HSIL. We don't know yet how many HIV+ women will get anal cancer over their lifetime. HIV+ women who have had other HPV cancers may also be at higher risk. So the bottom line is that anal cancer is rare in the general population, but for HIV+ people, anal cancer incidence is increasing as more people age with HIV.
Cervical cancer is also caused by HPV. If you look in the diagram above, the incidence of cervical cancer is now 7.8, but in the 1940's it was much higher, at 32.6. This 75% drop in cervical cancer incidence over the last 70 years is thought to have been the result of treating cervical HSIL after the Pap smear became a routine part of women's health care in the 1950's.
You're probably wondering, why don't we just do the same thing for anal cancer and start screening and treating everyone for HSIL? How could this be ethical? Screening to prevent cervical cancer in women began in the 1950s without any proof whatsoever that Pap smears and treatment of cervical dysplasia would help prevent cancer. It did as we see in the chart above. But we live in a very different health care environment today. To make a new screening test or surgical procedure a routine part of health care now requires evidence based on large clinical trials before they can be put into effect. The researchers behind the ANCHOR study been stuck in a catch-22 situation. We know that the precursor lesion HSIL exists. We know its treatment prevents cervical cancer, but the research funders, insurers and health care professionals need evidence that we can also prevent anal cancer this way. The only way to do this is to randomly assign participants to one of two groups, one treated and the other monitored, to see which group has the most cases of cancer. The ANCHOR study is designed to provide this evidence and to establish the standards of care to prevent anal cancer.
Further Reading:
- MJ Silverberg, et al. Cumulative Incidence of Cancer Among Persons With HIV in North America Annals of Medicine, Oct. 6, 2015.
- First HIV, then cancer. As people with HIV live longer, they are developing cancers at higher rates than the general population, Oct. 5, 2015, Mary Engel, Fred Hutch News Service.